Nursing documentation is a critical aspect of the nursing care workflow. There is a varying degree in how detailed nursing reports are described in scientific literature and care practice, and no uniform structured documentation is provided. This study aimed to describe the process of designing and evaluating the content of an electronic clinical nursing documentation system (ECNDS) to provide consistent and unified reporting in this context.
A four-step sequential methodological approach was utilized. The Minimum Data Set (MDS) development process consisted of two phases, as follows: First, a literature review was performed to attain an exhaustive overview of the relevant elements of nursing and map the available evidence underpinning the development of the MDS. Then, the data included from the literature review were analyzed using a two-round Delphi study with content validation by an expert panel. Afterward, the ECNDS was developed according to the finalized MDS, and eventually, its performance was evaluated by involving the end-users.
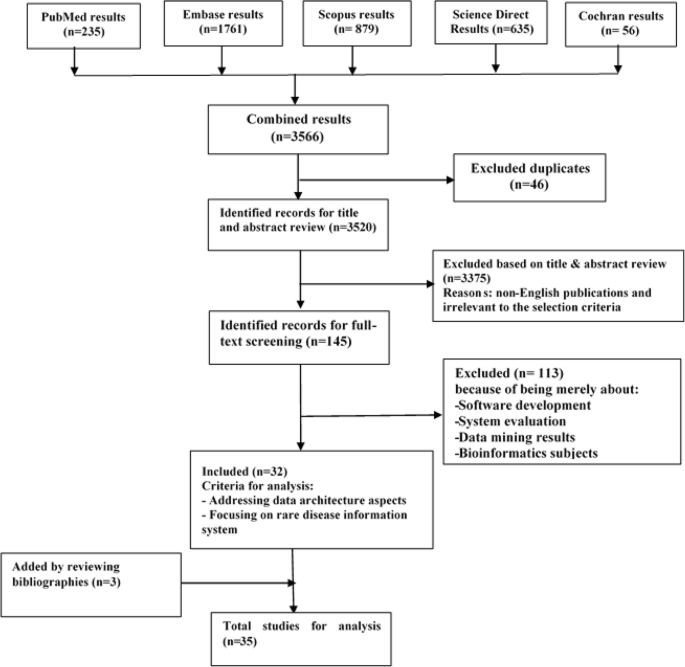
The proposed MDS was divided into administrative and clinical sections; including nursing assessment and the nursing diagnosis process. Then, a web-based system with modular and layered architecture was developed based on the derived MDS. Finally, to evaluate the developed system, a survey of 150 registered nurses (RNs) was conducted to identify the positive and negative impacts of the system.
The developed system is suitable for the documentation of patient care in nursing care plans within a legal, ethical, and professional framework. However, nurses need further training in documenting patient care according to the nursing process, and in using the standard reporting templates to increase patient safety and improve documentation.
Clinical documentation and access to reliable information are crucial facets of nursing decision-making in care practice [1]. Nurses and other caregivers aim to exchange information about patients and administrative activities with high quality standards such as precision, timeliness, concurrency, conciseness, comprehensiveness, organization, and confidentiality [2]. Nursing documentation is defined as written evidence demonstrating that the nurse’s authorized and moral responsibilities were met in order for care to be assessed [3]. Accurate and comprehensive documentation of nursing interventions is essential for several other reasons. It improves patients’ outcomes, increases the quality and safety of healthcare services, ensures practice accountability, and facilitates communication between various involved health care stakeholders [4]. Accordingly, the nursing documentation framework needs to be standardized, reasonably organized, and structured to mirror the phases of the nursing process, i.e., the assessment, diagnosis, planning, implementation, and evaluation of patient conditions [5]. Despite the importance of clinical documentation, currently, there are undesirable situations of care recordings and a lack of an appropriate framework for documenting nursing care [6]. Studies in Iran have revealed that the nursing documentation is not compliant with the standards. Several studies compared international standards with those reported in Iranian studies showed that nurses in other countries were more diligent in following documentation principles and standards [7]. Currently, the clinical nursing reporting in most hospitals in Iran is paper-based which may be similar to writing a story with a varied and inconsistent format. In most cases, there is no legislative defense for the nursing staff because of the gradual fading and illegibility of manual records [8, 9]. Writing a nursing report is a routine event that that should be performed several times during a nurse’s daily work, therefore, nurses spend about 37% of their entire working time writing reports [10,11,12]. One-half of all nurses must stay at work for 1–2 h after the end of their shifts, mainly to complete nursing records [13]. This approach has several drawbacks including wasted time, disruption in patient care, medical errors, endangering patients’ safety, fading and illegibility of the paperwork, high staff turnover rates, legal problems, and, other similar factors [14, 15]. Due to the fast developments in information technology, the health industry actively attempts to employ electronic medical records (EMRs) for clinical practice, research, education, and supervision purposes. The Nursing information system (NIS), as a module of EMR, control nursing care or services and manages the nursing activities through which data are assembled, exchanged, stored, extracted, presented, and transferred [16]. It has been revealed that employing an EMR and electronic clinical nursing documentation leads to higher quality, more complete, and more patient-centric documentation than manual nursing documentation. National Health information technology officials suggested the use of standard terminologies and data sets to enable interoperability across health information systems. Several terminologies exist that support nursing practice, but none have been broadly leveraged in Iran’s E-health system [17]. To comply with data standards, nursing specialists must decide which data items should be included in the context of patient care, and what required data could be documented by other healthcare staff [18, 19]. Therefore, to overcome the limitations of above-mentioned paper-based nursing documentation, some considerations must be addressed from a data management standpoint [20, 21]. Thus, the purpose of this study was to design, develop, and evaluate of an electronic clinical nursing documentation System (ECNDS) and determine its core data elements and the validity of their corresponding values.
A four-step sequential methodological approach was utilized. The minimum data set (MDS) development process consisted of two phases, as follows: First, a literature review was performed to attain an exhaustive overview of the relevant elements of nursing and map the available evidence underpinning the development of MDS. Then, the data included from the literature review were analyzed using a two-round Delphi study with content validation by an expert panel. Afterward, a web-based system with modular and layered architecture was designed based on the derived MDS. Finally, to evaluate the developed system, a survey of 150 registered nurses (RNs) was conducted and the positive and negative impacts of the system were identified.
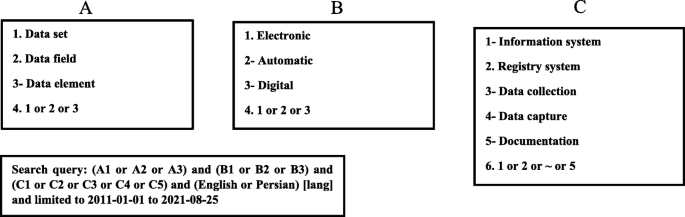
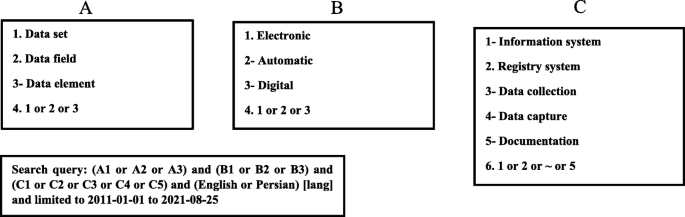
We performed a literature review to define the MDS-nursing report parameters. To conduct the study, first, an extensive literature review was performed in internet databases such as Web of Science, PubMed, ProQuest, Scopus, Magiran, and SID to identify the electronic nursing documentation system’s potential data elements. Thus, this step comprises all the elements associated with clinical nursing report templates and, it is necessary to incorporate and collect all elements related to nursing practices including diagnosis, assessment, and intervention. Inclusion criteria were (1) - availability of the full text of the journal articles, (2) - language (English or Persian), and (3) - publication date (from 2011 or later). Figure 1 shows the search strategy for identifying the relevant articles. The first part (Part A) included terms used for reporting templates. In the second part (Part B), the keywords related to digitalization were used. The third part (Part C) contained terms about studies on information system data architecture. The results of these three parts were combined using the Boolean operator “AND, OR”. The search was supplemented via checking the bibliographies of the identified articles.
Furthermore, previously developed relevant classification systems were systematically screened to collect information on clinical nursing report data elements, including the nursing diagnosis classification of the North American Nursing Diagnosis Association International (NANDA-I), and the Nursing Outcome Classification (NOC), Nursing Intervention Classification (NIC) and International Classification of Nursing Practice (ICNP). Finally, data fields were extracted from the related retrieved resources and entered into a checklist with two administrative and clinical sections.
The initial MDS content was validated by the Delphi technique using two rounds as bellow:
Using purposive sampling, we convened nursing professionals working as university faculty members of nursing in Iran’s Universities of Medical Sciences. Table 1 shows the demographic characteristics of these experts.
In this study, after searching in scientific databases and according to the processes provided by NANDA, CCC, and ICNP nursing classifications, we extracted a set of data elements and validated them via a two-round Delphi survey for inclusion in the final MDS of nursing documentation. We divided this dataset into three general categories, including the administrative category, nursing assessment, and nursing diagnoses. The number of participants in the Delphi stage was 80 subjects, including 74 individuals with a nursing Ph.D. degree, and six nurses with an MSC nursing degree. About 43% of the participants were female, 88% of them had more than 10 years of clinical experience, and all participants had an RN degree (Table 1).
This section has 19 items in our study. The items were delivered by the Delphi survey for nursing professionals. In the first round of Delphi, all the items of this section were confirmed (Table 2).
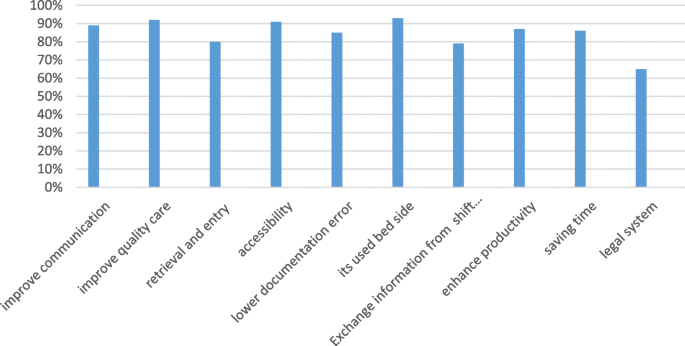
The ECNDS can improve the communication between departments (89% of the nurses who responded to the question on communication agreed that the system functioned well and nurses were satisfied with it). This system can also improve the quality of patient care (92%). By using it, the retrieval and entry of patient information become simple and accurate (80%). In addition, the system is easy to access (91%), and can be used by nurses in different wards (89%). It also reduces documentation errors (85%); and legal issues (65%). The developed ECNDS is utilized used at bedside (93%), facilitates exchanging information from shift to shift (79%), and boosts the productivity (87%) (Fig. 4).
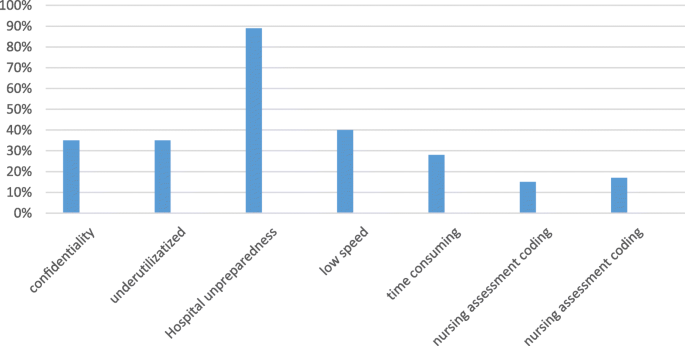
The second section of the survey is shown in Fig. 5 and describes the negative impacts of the ECNDS as follows: the loss of confidentiality (35% of the nurses answering the question on the confidentiality issue agreed that the ECNDS requires increased confidentiality); the ECNDS is dependent on utilities (35% of nurses agreed); the hospital is still using a paper system in some departments (89%); using the ECNDS is time consuming (28% agreed), and the system is works very slowly (60%). Moreover, 17% of the participants disagreed with the validity of coding the nursing diagnosis and 15% of them disagreed with the validity of the coding of the nursing assessment.
The field of information technology is developing and with its progress, it can help the advancement of other sciences such as nursing science. In Iran, nursing documentation is still conducted in a traditional and paper-based manner [8]. Electronic clinical nursing documentation needs the data to be stored according to a uniform and structured framework. This study aimed to design an electronic clinical documentation system for unified recording of nursing activities using standardized data elements which improve data quality, data interoperability, and decision-making, and pave the way for formulating global standards for nursing care. In this study, we conducted a systematic review study along with a two-round Delphi survey to prepare a formal and organized data structure and standard platform. This MDS could be applied to develop more patient-oriented, evidence-based, safe and high-quality nursing care. The developed MDS also helps to support decision-making. After the survey, the system was found that it prevents 65% of the legal issues, reduces 85% of documentation errors, and does not have the problems of the paper documentation process. After using the system, 92% of the nursing staff were satisfied with the increase in the quality of care, which is in line with a study in Oman [27]. In Iran, nursing documentation is a paper-based approach, and nurses spend about one to two hours completing nursing reports [28]. However, in this survey, 82% of the nurses stated that their time was saved by utilizing the system developed in this study. In our study, nurses’ satisfaction with filling nursing report documentation at the patients’ bedside, and exchanging information from one shift to another shift were 93 and 79%, respectively [12]. In other words, filling or documentation of the clinical nursing report at the patients’ bedside and exchanging patient information across shifts are two important features of a nursing report that were taken into account in our designed system. The ability of software to keep the information confidential is one of the most fundamental features of this tool. Due to the team’s support for its security, the system designed in our study received 65% satisfaction from nurses.
We discovered the benefits and drawbacks of EMR systems, from reviewed studies, e.g., equipment shortages and breakdowns, writing on paper and transferring to EMR [29], user-friendliness and interoperability, hardware and software problems, increased documentation load, lack of formal structure, inability to use at bedside, and other factors [30]. Therefore, in the system developed in our study, the following features have been considered to solve the major problems of EMR. Unlike other studies, our work has a formal and organized structure according to the nursing process, which has been shown to improve legislative compliance and completeness nursing documentation completeness [27, 30]. Our software indicated that with the advancement of EMR in nursing practice, many paper-based reporting problems such as; wasted time, disruption in design and clinical care the patients, medical errors, endangering patients’ safety, fading and illegibility of manual documentation, legal problems, and, other similar issues. Are resolved [8, 9]. The electronic system developed in this study allows the nurses to fill out the pre-designed standard platform at the patient’s bedside, eliminating the need to write on paper and transfer the information to the system. One of the time-consuming and non-user-friendly problems of EMR systems is recording reports on paper and transferring them to the system [29], which was solved in our software. On the other hand, this process is recorded at the patients’ bedside, and therefore, the patient’s information is not missed. Moreover, our software shows a graph of the progression of a patient’s clinical conditions such as the patient’s heart rate in different shifts. The mentioned features are among the strongest aspects of this system, which have been stated in a survey of clinical nurses. The simplicity and fluency of the designed platform as well as the existence of scientific and approved abbreviations in this platform are another advantage of this software noted in the survey by the nurses. Another key feature of this system is that it can be used in general and specialized clinical wards such as CCU. In the survey, nurses emphasized the software security factor in maintaining patient information and the support team of this system, which is a very important aspect in any software. Finally, we must mention that our designed software has the following features; (1) the existence of an official structure and approval by nursing professors; (2) it can be used in all hospitals and different wards;(3) it can be easily used in the bedside; (4) it has the ability to report nursing information from shift to shift; (5) after a survey of nurses working in the wards of Abadan hospitals, it was concluded that our system is user friendly, easy to learn and easy to used.
This study should have been used in more hospitals with more nurses; on the other hand, nurses were because of the heavy workload of nurses in clinical wards and their lack of spare time, it was difficult for them to participate in this study. In addition, nurses needed training use this system, took great effort. The infrastructure of some hospitals was not suitable for the components of this design and it was very challenging to build the necessary infrastructure.
The primary purpose of the nursing documentation MDS was to scientifically reduce the amount of clinical nursing report data collected and documented by nurses during the patient care process, while also enhancing the enjoyment of nursing due to a reduction in documentation burden. Involvement of the system end-users in a meaningful way during the development process resulted in an easier conversion from paper-based to computerized documentation, higher approval from nurses who use the electronic nursing documentation system, and minimal complaints regarding its content in the practice setting.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.